Medical practices that leave money “on the table” as a result of billing inefficiencies should correct these inefficiencies and now.
One of the most common operational language clauses in payer contracts is referred to as the “lesser of billed charges” clause. The clause is usually worded like this: “[Payer] will pay provider the lesser of its billed charges or its payer contracted rate for each CPT® code’s reimbursement.”
What does this mean exactly and why is it important?
What this means is that, for example, if your payer contracted rate is $110 for CPT® code 99213, but your billed charge is $90 for this code as defined in your charge master, you will be paid $90 per office visit rather than $110, your contracted rate!
The common response is; “not us, we double the Medicare Rates and use that as our charge master.”
At least that’s the response until we show them otherwise.
We are going to run a series of analyses, showing the most commonly under billed CPT® codes by specialty. 1st up – Dermatology.
Stay tuned, your specialty coming soon.
DERMATOLOGY
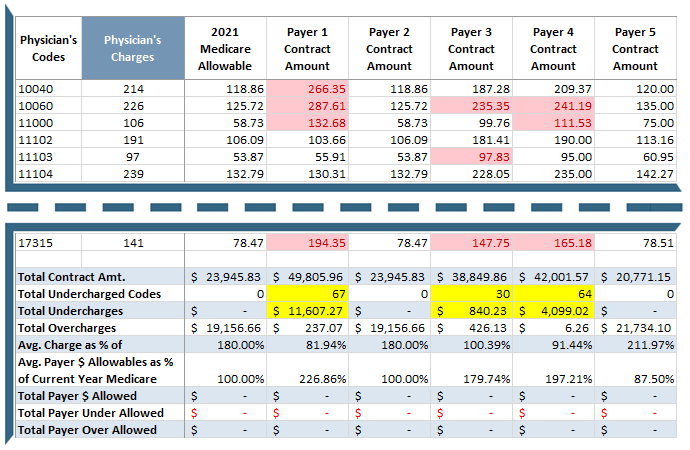
Sample Size: (AL, GA, FL, MS and SC), 2 small to mid-size dermatology practices from each state, 10 total, actual clients, weighted average. They each had ~200 CPT® codes in their charge master. We looked at codes 10040 thru 17315. They had not looked at their charge master in a number of years.
This is what happens when payer contracts and fee schedules are not given the attention they require.
Note: CPT® codes, specialty and numbers will change. We hope you get the point, every dollar counts!
Think About This
It would be virtually impossible to negotiate a new contract based on the above data. The payer believes you are satisfied with the rate(s) because your charge is not even meeting the current rate(s). The good news is that this is fixable.




