BASICS OF VALUE-BASED CARE
The patient reimbursement model plays a crucial role in patient satisfaction, physicians are always trying to improve the patient experience by reducing the cost of service. Most physicians use a fee-for-service (FFS) model, which incentivizes them based on the number of services provided instead of the quality of care.
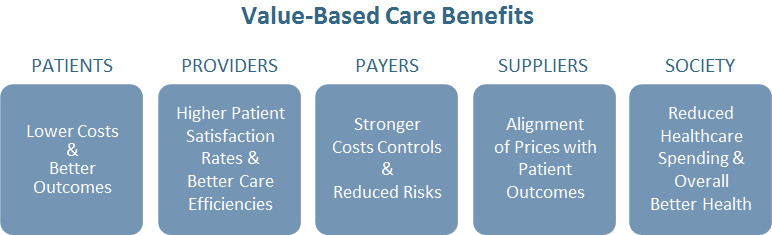
Value-based care seeks to change the way patients receive healthcare, ultimately resulting in various benefits for everyone involved. In this article, we explain what Basics of Value-Based Care is, how it’s different from traditional reimbursement models and how both your patients and your practice can benefit from adopting a value-based healthcare model.
WHAT IS VALUE-BASED CARE?
Value-based healthcare is a pricing model that incentivizes your practice based on the quality of services you provide to patients. Within a value-based care model, your practice is compensated depending on a patient’s health outcomes.
On the other hand, the traditional FFS model pays based on the number of visits, tests performed, services performed, etc. Value-based care puts more emphasis on taking care of patient’s medical needs in as few visits as possible and to the best of the physician’s ability. Value-based care tries to: improve the quality of healthcare; improve the patient experience; lower costs for patients and improve the care team’s experience.
Under FFS models, physicians are paid per service, which means the more tests and procedures they prescribe to patients, the higher they get paid. Since the focus is on the number of services, patient care tends to get ignored. Physicians spend less one-on-one time with the patients and prescribe more tests without getting to the root of what patients may be experiencing, thus impacting the overall health outcome.
Value-based care is driven by data; as physicians have to track and report specific quality metrics to demonstrate improvement in patient health outcomes. Things such as hospital readmissions, adverse events, population health, and patient engagement during treatment are some of the metrics evaluated.
MAIN TYPES OF MODELS
Accountable Care Organization (ACO): An ACO is a network of doctors, hospitals, and other providers that works together to offer coordinated care to patients. Under this type of value-based care, network providers share in the savings if the ACO is able to provide adequate care and high-quality services that reduce healthcare costs for patients. If the ACO provides excellent care and services, everyone shares in those cost savings, but if care quality isn’t adequate, providers in the network may have to repay payers for not delivering better care.
Bundled Payments: Bundled payments allow payers to pay a single price for the services delivered during the patients entire episode of care, even if multiple providers have treated the same patient during an episode. The payment is bundled because all physicians, settings of care, and procedures are paid out together based on the treatment outcome.
Patient-Centered Medical Home (PCMH): The Patient-Centered Medical Home (PCMH) is a care delivery model whereby patient treatment is coordinated through their primary care physician to ensure they receive the necessary care when and where they need it, in a manner they can understand.
The objective is to have a centralized setting that facilitates partnerships between individual patients, and their personal physicians, and when appropriate, the patient’s family. Care is facilitated by registries, information technology, health information exchange and other means to assure that patients get the indicated care when and where they need and want it in a culturally and linguistically appropriate manner.
WHAT IS VALUE-BASED PAYMENT (VBP)?
The United States healthcare system is rapidly moving toward rewarding value over volume. Legislation, such as the Affordable Care Act and the Medicare Access and CHIP Reauthorization Act (MACRA), solidified the role of value-based payment in Medicare programs.
The VBP model for medical services is gradually replacing the traditional fee-for-service (FFS) model for payers and healthcare organizations. The goal is to cut rising healthcare costs by switching from a fee-for-service based model based on quantity to a value-based model based on quality.
In contrast to the predominant FFS model, in which payers reimburse physicians a fixed fee for each service they provide from an approved list, VBP models hold physicians financially accountable for both the cost and quality of care they deliver. VBP models reward physicians financially for delivering better, more cost-effective care and can penalize them for failing to do so.
The VBP model is one approach to achieving a balance between efficiency and effectiveness and comes in different forms, varying in the level of physician accountability. The level of payment a physician receives is tied to cost and quality targets. These targets ensure that physicians do not cut costs at the expense of patient outcomes. These targets are achieved through measured performance.
VBP models support a three-part aim:
- Better care for individuals
- Better health for populations
- Lower cost
VBP CALCULATIONS
VBP programs reward healthcare providers with incentive payments for the quality of care they give to people. VBPs are calculated by using numerous measures of quality and determining the overall health of populations.
Unlike the traditional FFS model, value-based care is driven by data; providers must report to the payer on specific metrics and demonstrate improvement. Physicians may also have to track and report on hospital readmissions, adverse events, population health, patient engagement, and more.
Under the new models, physicians are incentivized to use evidence-based medicine, engage patients, upgrade health information technology, and use data analytics to get paid for their services. When patients receive more coordinated, appropriate, and effective care, providers are rewarded.
To participate in value-based care, payers have developed several models for physicians, including Accountable Care Organizations (ACOs), bundled payments, and Patient-Centered Medical Homes (PCMH).
WILL VBP MAKE A DIFFERENCE?
Value-based care is cited as one of the best ways to reform healthcare, stakeholders say. VBP is a catchall term for ACOs and other modes for restructuring healthcare around a system that puts more weight on quality metrics or the aggregate health of a population rather than how many visits someone makes to the hospital or how many procedures one has. The intent of the system is to maximize value for patients and define health outcomes achieved per unit of cost spent.
As we move forward, VBP models provide new opportunities for the development and participation of ACOs. The Affordable Care Act is promoting the use of ACOs and levies penalties for hospital readmissions to encourage better follow-up care outside the hospital. It is a more data-driven vision of healthcare reform that not only improves quality and efficiency but also reduces costs.
VALUE-BASED CARE IS THE FUTURE
Value-based care is becoming more and more popular because of the incentives payers and the government are offering physicians to make the change. With new legislation being passed, more providers are expected to make the shift and realize the benefits a value-based care model can give to their practice and patients. One of the key challenges practitioners face is effectively tracking the metrics required to determine ‘value’ in a value-based model. A healthcare organization will need to track staffing data, time and attendance of patients, clinical data, patient acuity data, and a bevy of other things to determine how to calculate the cost of healthcare.




