You need to have the tools that will illuminate the added value your organization provides to their members. Remember that you are providing a valuable service to their organization and it is important that you remind them of this often-forgotten fact.
Considerations During the Prenegotiation Phase
These questions (but not limited to) should be incorporated into your Contract Renegotiation Notice. It would be a mistake to simply state “you want more”, you must make your case. If true, it should be stated that you have not had an increase to your reimbursements in (x years).
- What separates you from your competition?
- What do you do clinically better than your competitors?
- What benefits do you bring to the hospitals you cover?
- What are benefits to the patients you treat; what is the level of patient satisfaction?
- What do you do clinically that reduces healthcare costs for the payer?
- What about you makes you “special” within the payer’s provider network?
The success of renegotiation rests on the ability to provide cost-effective, evidenced-based services and convince payers of their value! The goal is to tell a story about the practice and communicate why a raise in rates should be granted. Your purpose is to convince the payer that you offer superior service, above and beyond what other competitors offer.
Understanding and Defining Your Leverage
The ability to negotiate or renegotiate a managed care contract is often determined by the amount of leverage a practice or provider has in the marketplace. To identify your negotiation leverage (or lack thereof) and opportunities for shared benefit, start with a SWOT analysis (strengths, weaknesses, opportunities, threats). Most physicians come to the negotiation table without a defined contract strategy.
Creating an Effective Payer Proposition Letter
Your CodeToolz Contract Analyzer provides the kinds of data you need prior to negotiating reimbursement rates with payers. Now it is time to put this information to work by preparing a simple but substantive proposal letter that is sent to the payers’ contracts manager that introduces the practice, the request for a rate increase and, most importantly, the reasons for the proposed increase.
An effective letter is no more than one to 1½ pages long. Remember that this letter is a sales pitch and attention getter, written from the perspective of payers explaining to the latter why they should increase your reimbursement. Payers need a good reason to give you more money.
Initial Payer Responses
You can expect most payers’ initial response to inform you of a moratorium on negotiation or a “we’re already paying market value” message. Don’t accept that. Tell them that’s not in the contract. If the payer is not willing to publish the fees it pays other practices (and they’re not), its claims about market value to other practices will be unsubstantiated and meaningless to your negotiation. Our Contract Analyzer determines what other payers are paying in your market.
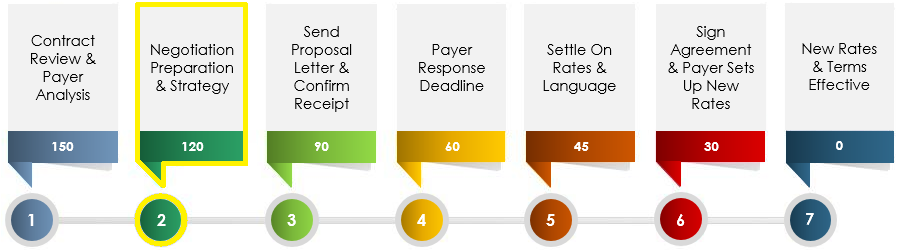
Timeframe for Completion
The timeframe for the completion varies by area and the cooperation of both the insurance companies and respective client. Typically, clients can expect anywhere from ninety days to six months. Constant dialogue is needed for the contract negotiations to be successful.
Executive Summary
Ensuring maximum reimbursement is always at the top of a healthcare provider’s mind. But we find too often that many providers are leaving money on the table with inefficient and infrequent payer contract management.
Let the experts at CodeToolz take your contracting efforts from burden to competitive advantage. The bottom line is that in negotiations, knowledge is power and planning is essential.




