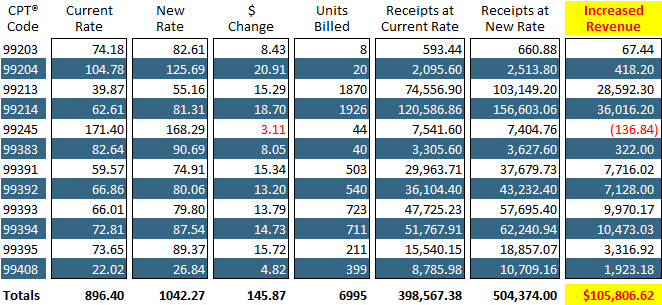
Most offices have never renegotiated their contracts and very few renegotiate them on an annual basis, missing out on additional revenue that can be substantial and greatly impact the practice’s revenue.
With your CodeToolz Contract Analyzer, your Contract Renegotiation Notices are automatically created for you, based on anniversary date – no more outdated fee schedules.
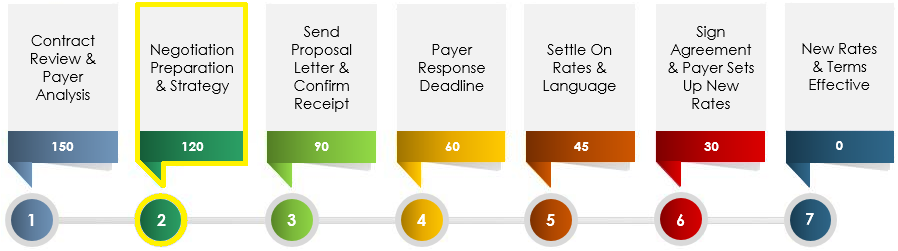
Payer Contract Renegotiation Process and Timeline